SPARX3 in PD
Sparx3 is a national trial investigating the impact of exercise on the management of Parkinson’s Disease. While Parkinson’s management is typically multimodal, involving both exercise and medical therapy, this trial isolates the effects of exercise alone. It aims to evaluate the attenuation of Parkinson’s symptoms after 12 months of high-intensity versus moderate-intensity exercise, before any exposure to medical therapy. We are currently recruiting individuals who have recently been diagnosed with Parkinson’s Disease and have not yet undergone any medical treatments.
BFR and IRT in PD
Falls are a common predicament for individuals with Parkinson’s disease (PD) due to poor balance, which is hard to treat with regular medication. Weak leg muscles also contribute to poor balance and frequent falls in PD. We think a combination of two exercises—Blood Flow Restriction (BFR) and Instability Resistance Training (IRT)—could help improve balance and muscle strength in people with PD. This study will last six weeks, with progress checked before and after the intervention as well as six weeks following the last visit. We’ll measure how well participants adhere to the program, side effects, changes in balance, strength, mobility, quality of life, and other health factors. Our long-term aim is to create better treatments to help people with PD stay steady and slow down the disease’s impact.
Past Projects
BFR and knee OA
Knee osteoarthritis often limits a person’s ability to tolerate high resistance exercises necessary to improve muscle strength. This is especially relevant in the context of postoperative recovery from total knee replacement surgeries for individuals with osteoarthritis. This study will evaluate if physical therapy at lower intensities with blood flow restriction prior to surgery can be a means to feasibly increasing muscle strength in this population without the same demand.
AE and VR in PD
Exercise has been shown to be an effective primer to rehabilitation and facilitates neuroplasticity. In this study we are analyzing how different intensities of exercise can impact balance, postural control, and neuroplasticity in Parkinson’s Disease. We are comparing neuroplasticity, blood-based biomarkers, spinal reflex excitability, balance, and gait before and after the completion of the intervention.
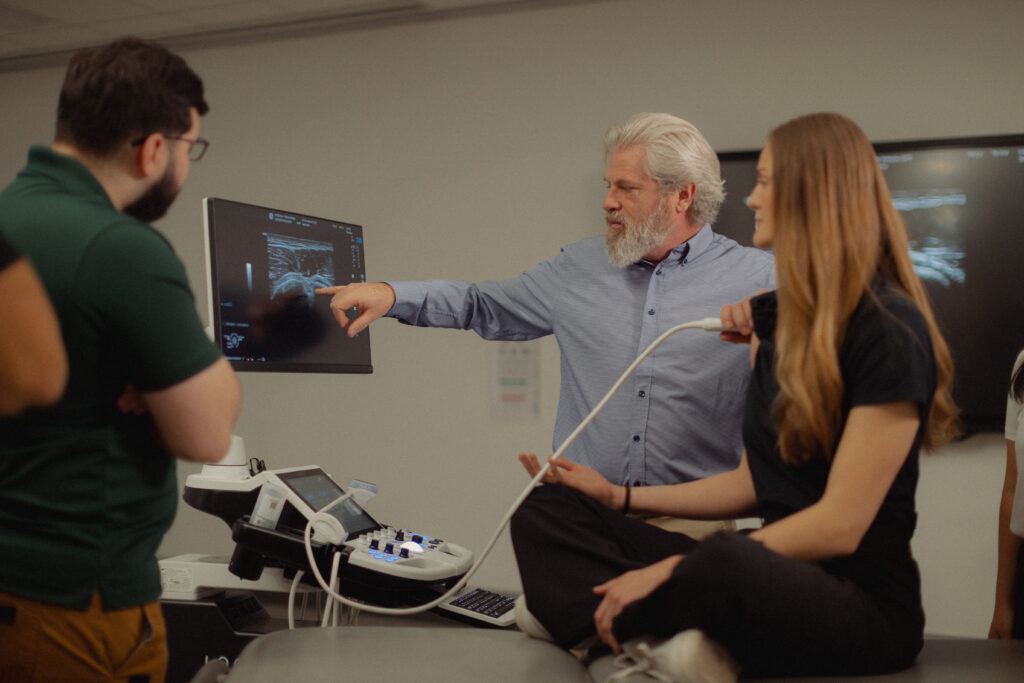
EMIMSK
The EMIMSK Study is exploring how two preventive treatments—traditional factor VIII infusions and the newer therapy emicizumab—affect joint and bone health in people with severe Hemophilia A. Using point-of-care musculoskeletal ultrasound imaging to allow detailed measurement of joint damage, researchers will follow participants over three years to determine which approach offers better long-term protection, mobility, and quality of life